Illinois residents who are eligible for Medicare and Medicaid coverage and benefits can get it all through Humana Gold Plus® Integrated Medicare-Medicaid in Illinois. Through Humana Gold Plus Integrated, your Medicare and Medicaid coverage and benefits are combined into one plan—PLUS you get prescription drug coverage.
Humana Gold Plus Integrated Medicare-Medicaid in Illinois

Helping you on your journey to good health
We believe everyone should be able to achieve their best health. Healthcare may seem complicated, but by working together, we can simplify it for you. Our members with Humana Gold Plus Integrated get personalized support from people who care.
Get ready to renew your Medicaid coverage
Illinois is checking to make sure you are still eligible for Medicaid coverage. To ensure a review of your Medicaid coverage, please update your information with the state:
- Visit
abe.illinois.gov and select “Manage My Case.” - Verify your mailing address under “Contact Us.”
- Locate your due date (the “redetermination” date) in your “Benefit Details.” You can opt-in for text and email alerts about your renewal date. Select the “Account Management” tab under “Manage your communications preferences.”
Everyone’s renewal date is different, so it is critical that you get ready to renew.
You will receive renewal information in the mail about 1 month before your renewal date. Please complete and return it right away.
For help with your renewal, call 800-843-6154.
Beware of scams. Illinois never will ask you for money to renew or apply for Medicaid. If someone reaches out to you asking for money to renew or apply for Medicaid:
Report the scam to the fraud report website ,- Call the Medicaid fraud hot line at 844-ILFRAUD (453-7283)
Coverage
Our members with Humana Gold Plus Integrated get:
- Annual well visits with $0 copayment
- Annual breast cancer screenings with $0 copayment for women age 40 and older
- Tobacco-cessation services
- Emergency care with $0 copayment
New member information
Welcome to Humana Gold Plus Integrated. We get to know the unique needs of our members and our communities, and together, we create solutions to help people reach the best version of themselves.
From time to time, Illinois Medicaid sends Medicaid recipients in Illinois information in the mail. To make sure you get this information, Illinois Medicaid must have on file your address. Updating your address with Illinois Medicaid is easy:
Connect with Illinois Medicaid online - Call 877-805-5312 (TTY: 877-204-1012), Monday – Friday, 7:45 a.m. – 4:30 p.m., Central time
If Illinois Medicaid does not have a current address on file, you may lose your health coverage.
Go365 by Humana
Our members can enroll in Go365 by Humana™ and earn rewards for completing health actions.
Enrollment information
You can enroll into Humana Gold Plus Integrated when you are newly eligible for Medicare and Medicaid coverage or if you have a different plan and want to switch plans.
Consumer Advisory Committee
Humana Gold Plus Integrated members can join and participate in our Consumer Advisory Committee. Participants can give us feedback on how well we’re doing as a health plan.
Extras from Humana
Humana Gold Plus Integrated members have access to benefits to help you make the most of your plan
Coverage area
We are proud to provide coverage statewide in Illinois for people eligible for Medicare and Medicaid.
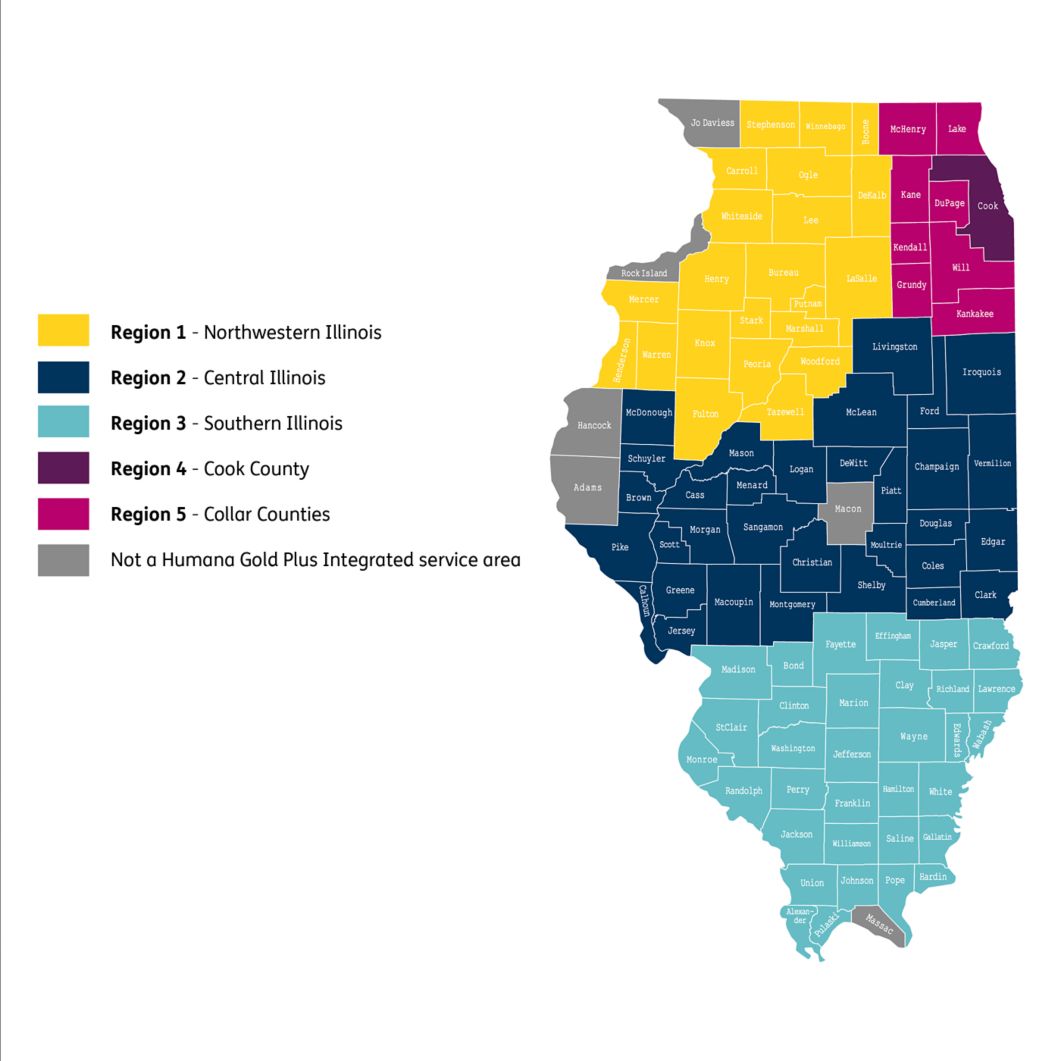
Humana Gold Plus Integrated coverage area
Get more information about
File a grievance or appeal with the
Humana Gold Plus Integrated may terminate or not renew its contract or decide to reduce its service area. The effect of any of these actions may affect your benefits and/or enrollment.
Humana Inc. and its subsidiaries comply with all applicable federal civil rights laws and do not discriminate on the basis of race, color, national origin, ancestry, religion, sex, marital status, gender, gender identity, sexual orientation, age, or disability. See our full accessibility rights information and language options.