Say no to the flu. A yearly flu vaccine is recommended for everyone 6 months and older. Get yours today!
Humana Healthy Horizons in Florida
When you choose Humana Healthy Horizons® in Florida, you get Medicaid that does more. We give you what you need to feel your best, plus things that you didn’t even know you needed. We call that human care.

Helping you on your way to better health
Humana Healthy Horizons in Florida is proud to partner with the Florida Agency for Health Care Administration (AHCA) to provide Medicaid coverage to eligible Florida residents through managed medical assistance (MMA) plans. We are committed to improving health for all Floridians.
With Humana Healthy Horizons, you get Medicaid that provides you with the everyday benefits, rewards, and support that make your life easier so that you have time to focus on what you love.
Humana Healthy Horizons in Florida coverage area
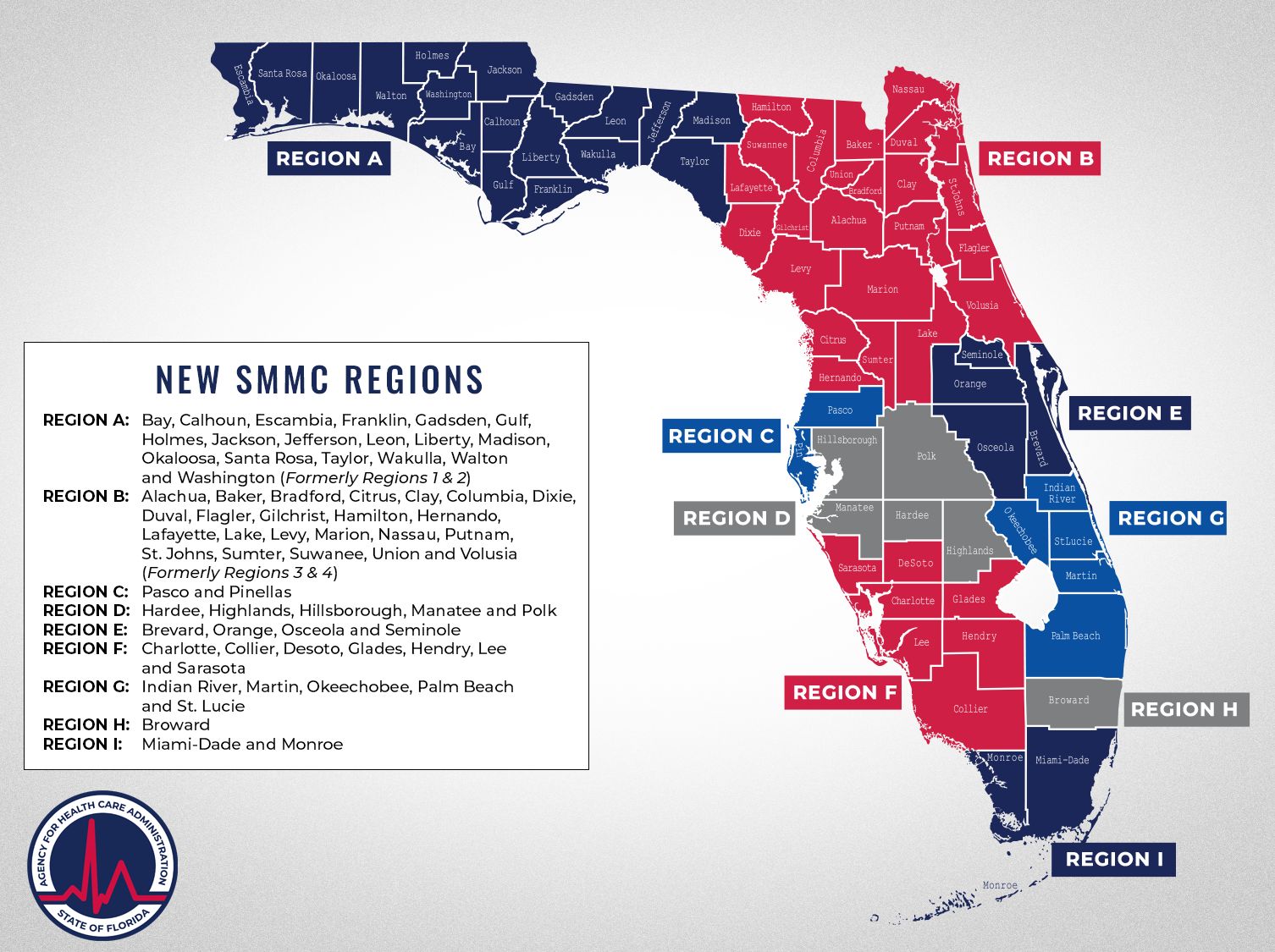
Florida SMMC coverage regions
Region A: Bay, Calhoun, Escambia, Franklin, Gadsden, Gulf, Holmes, Jackson, Jefferson, Leon, Liberty, Madison, Okaloosa, Santa Rosa, Taylor, Wakulla and Washington
Region B: Alachua, Baker, Bradford, Citrus, Clay, Columbia, Dixie, Duval, Flagler, Gilchrist, Hamilton, Hernando, Lafayette, Lake, Levy, Marion, Nassau, Putnam, St. Johns, Sumter, Suwannee, Union and Volusia
Region C: Pasco and Pinellas
Region D: Hardee, Highlands, Hillsborough, Manatee and Polk
Region E: Brevard, Orange, Osceola and Seminole
Region F: Charlotte, Collier, DeSoto, Glades, Hendry, Lee, and Sarasota
Region G: Indian River, Martin, Okeechobee, Palm Beach and St. Lucie
Region H: Broward
Region I: Miami-Dade and Monroe
Humana Healthy Horizons in Florida
Looking for help?
Contact Us
If you have questions, find the number you need to get help and support.
Find Care
Find a doctor, hospital, or pharmacy.
Documents and forms
Find the documents and forms you need, including your member handbook.