When you choose Humana Healthy Horizons® in Florida, you get Medicaid that does more. We give you what you need to feel your best, plus things that you didn’t even know you needed. We call that human care.

Helping you on your way to better health
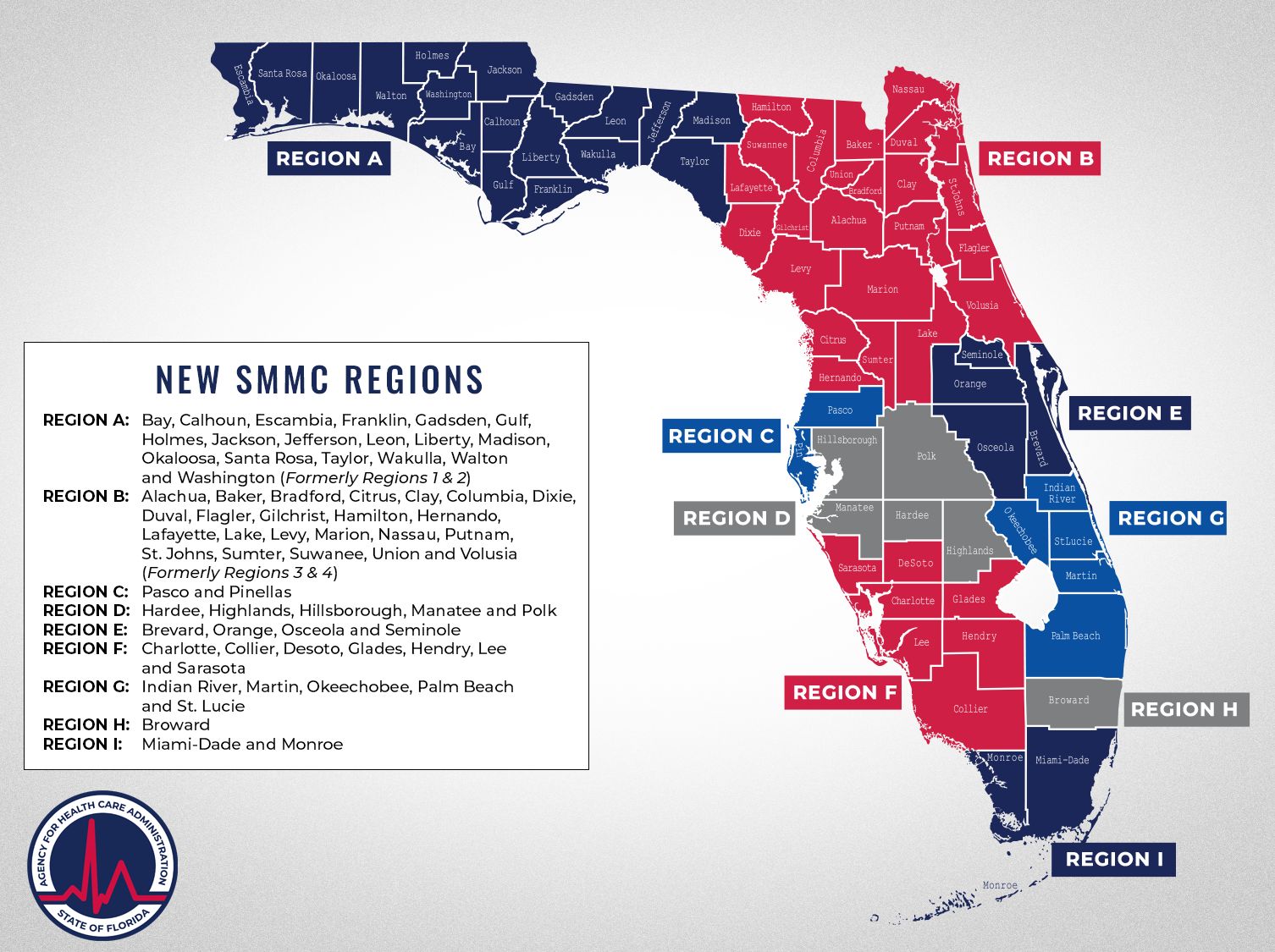
Humana Healthy Horizons in Florida is proud to partner with the Florida Agency for Health Care Administration (AHCA) to provide Medicaid coverage to eligible Florida residents through managed medical assistance (MMA) plans. We are committed to improving health for all Floridians.
With Humana Healthy Horizons, you get Medicaid that provides you with the everyday benefits, rewards, and support that make your life easier so that you have time to focus on what you love.